_htm_cmp_blends110_bnr.gif)
We've already discussed the basics about bunions on a separate web page. That web page included some information on conservative, non-surgical treatments, but when those conservative treatments fail, it may be time to consider surgical intervention. The purpose of this web page is to discuss some of the basic surgical procedures that exist to correct painful bunions, if the prospect of surgical intervention is entertained.
To start, in order for you to understand what is presented on this web page, it's important to review our web page on how bunions are evaluated on X-ray, as several terms used on this page (like Intermetatarsal Angle, Hallux Abductus Angle, and PASA) are discussed there in some depth, and it may be difficult to understand what's discussed here without understanding those concepts.
When conservative measures
fail and you wish to try surgical options, how do you do the
procedure?
Many people think that a bunion surgery consists simply of lopping off the bunion bump. In fact, most people use terminology to suggest this by saying, "I need to have my bunion removed."
But surgical correction of bunion deformities can be accomplished in a surprisingly large number of ways. In fact, there have been more than 100 procedures described to correct a bunion. And while the bump of a bunion is typically removed during the surgery, the majority of surgical procedures emphasize more in the way of the realignment of the bones.
While no means a comprehensive list of the techniques available to correct
this deformity, we've tried to compile a list of procedures in a variety of
categories that represent
common examples of procedures that are most likely to be be chosen, or
procedures that are widely-known, even though they may not be done much any
more.
In
order to manage the list of procedures discussed on this web page, we've divided
the procedures into several categories:
-
Bump Removal Procedures (procedures involving just the removal of an enlarged "bump" of bone.)
-
Head Osteotomies (procedures involving a bone cut near the great toe joint)
-
Shaft Osteotomies (procedures involving a bone cut in the shaft of the metatarsal bone)
-
Base Osteotomies (procedures involving a bone cut at the far end of the metatarsal bone)
-
Procedures Proximal to the First Metatarsal (procedures performed into the midfoot)
-
Joint Salvage Procedures (procedures that attempt to salvage the great toe joint when severe arthritis is present)
-
Joint Destructive Procedures (procedures that require destruction of the great toe joint)
-
Soft Tissue Procedures (procedures that primarily involve the soft tissues only)
-
Digital Procedures (procedures usually done in tandem with other surgeries)
-
Combination Procedures (combinations of more than one procedure)
Bump Removal Procedures
The procedures in this category are
chosen when there is an enlarged bony bump around the great toe joint.
These procedures may be chosen alone, although they are done so rarely because
simple bump removal does not address the reason the bump formed in the first
place. Hence, the deformity often tends to return.
Silver
This
procedure involves removal of the enlarge bump on the side of the
foot. It may also be known as an exostectomy.
As most bunion deformities have an enlarged bump, this is done
as part of most bunion surgeries--but not done frequently by itself, as it
doesn't address the cause of the deformity or allow for any straightening of
a misaligned toe or joint.
| McBride Procedure
This
procedure involves performing a Silver procedure (described above), but it
adds the surgical release of a tendon that holds the great toe in
its "crooked" position. McBride procedures are
usually only chosen in early bunion
development, or in cases where a cut in the bone is not advised for
some reason. McBride surgeries heal very quickly, but they do
not address the cause of the complaint particularly well, and
bunions are more likely to return following this procedure compared
to other procedures. |
 |
Cheilectomy
This
procedure involves removal of the bony bump on the top of the big toe
joint. (See web page on
Hallux
Limitus and
Hallux
Rigidus.) Used frequently for cases with mild to moderate
arthritic change in that area, but frequently done in combination with other
procedures, as it doesn't address the cause of the bump on the top of the
joint.
Head Osteotomies
The procedures in this class are all designed such that a bone cut (osteotomy) is made in the region of the first metatarsal known as the head, which is located just behind the great toe joint. Most procedures in this class are designed to address a moderate degree of abnormality in the Intermetatarsal (IM) angle that accompanies most bunion deformities, the deviated cartilagenous surface (known as the PASA), or both.
Osteotomies performed in this region of
bone are relatively fast-healing, and many allow for immediate post-operative
ambulation.
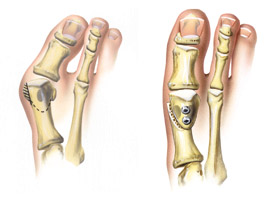
Though Austin initially described this procedure without any fixation (pins, wires, screws), it is usually performed with fixation today.
|
|
 |
But because they afford more stability, screws are superior forms of fixation. And while not impossible to use screws with the Austin procedure, (as you can see on the left), other procedures do offer easier and more stable screw fixation. (We'll discuss some of these procedures below.) Because of its interlocking pieces, this procedure usually allows for immediate post-operative ambulation, which is a huge advance compared to how earlier procedures were performed. |
| Kalish Procedure
or Offset
V Procedure
Developed by a podiatrist
in Georgia named Dr. Stanley Kalish, this variation of the Austin
procedure involves a similar V-shaped cut
in the metatarsal bone, but this is made with a long arm on
the top of the bone to allow for easier screw fixation. |
|
Adding small additional bone cuts allows one to shorten or drop (plantarflex) the metatarsal.
There are few downsides to this procedure when compared to the Austin procedure, other than the fact that somewhat more tissue dissection is required to make this bone cut.
Plantar V Procedure or Plantar Wing Offset V procedure is basically an inverted Kalish procedure--with the long arm directed on the bottom of the foot. This procedure has pretty much the same advantages as the Kalish, but there are a couple of downsides. First, it's slightly more difficult to visualize the pieces and screw fixation when the wing is placed on the bottom. Second, testing has shown that a wing on the bottom of this procedure is somewhat more likely to cause cracking of the "wing" portion of the bone cut, making it somewhat less stable than the original Kalish. Further, there is no inherent advantage to making the wing on the bottom, so this procedure is less frequently chosen for these reasons.
| Youngswick
Procedure Devised by a
California podiatrist named Dr. Fred Youngswick, this common modification to the
Austin Procedure requires an additional wedge of bone to be taken from the
upper of the two "V" cuts, allowing the surgeon to not
only address the IM angle, but to shorten and drop the metatarsal
head as well. This procedure is chosen in
cases where moderate arthritis and limitation of motion is developing at the great
toes joint, or when the metatarsal is abnormally long or elevated. This procedure can also be performed with a Kalish
modification, to allow for easier screw fixation. An
excellent procedure in the right applications. |
| Reverdin Procedure
The original Reverdin procedure was first described in 1881. Its aim
was to reorient the cartilage surface of the 1st metatarsal. The
procedure involves removing a triangular-shaped bone cut from the top of the
1st metatarsal. When the triangular-shaped fragment is removed, the cartilagenous joint surface
(PASA) is rotated into its corrected position relative to the toe. The
major downsides of the classical Reverdin are that it is unstable, difficult
to fixate, and the bone cuts can compromise the two bones beneath the 1st
metatarsal, the sesamoids.
While the Reverdin procedure is rarely done
in its classical form for these reasons and would otherwise have been
relegated to the "historical procedure" bin, several modifications
to the Reverdin procedure have been described to overcome its
disadvantages. Thus, the Reverdin, in modified forms, have maintained
the Reverdin as a very versatile and very popular procedure. |
| For example, to better protect the
sesamoids, to increase stability and to allow for screw fixation, the Reverdin-Green
was devised in 1977. It involves the same basic bone cut as the
Reverdin, but a shelf of bone is created on the bottom (plantar
portion) of the metatarsal head. This procedure is also
known as the "Distal
L" procedure,
because of the appearance of the bone cut.
This procedure addresses PASA (the joint deviation) only. |
 |
However, simply by taking the same Reverdin-Green bone cuts and sliding the head of the bone towards the lesser toes before fixation is inserted allows you to address both the PASA and the Intermetatarsal angle to be corrected at the same time. This modification is known as the Reverdin-Green-Laird. This is a very commonly-chosen procedure.
| To allow the head of the bone to be lowered, we also have the Reverdin-Green-Laird-Todd procedure. In this procedure you start with the Reverdin-Green-Laird procedure, but an additional triangular-shaped wedge is also removed from the operative site, allowing the surgeon to address the bunion in three dimensions. You can correct PASA, the metatarsal angle, and an an abnormally-elevated metatarsal bone. An example of how the bone is lowered following this procedure is demonstrated on the x-ray to the right. |  |
Another variation of the Reverdin is the Crescentic Reverdin or Arcuate Reverdin procedure. This is performed in the same area as the standard Reverdin, but it involves a C-shaped bone cut to rotate the cartilage into place. One big advantage to this procedure over the traditional Reverdin is that it does not involve removing a wedge of bone, and so it does not shorten the bone. This procedure is most frequently performed with the "Green" modification to help protect the sesamoids, increase stability, and allow for better screw insertion.
DRATO Procedure This versatile procedure probably allows for more different forms of correction than any other. It is performed by making a vertical cut in the metatarsal head. This allows the head to be rotated in order to allow misaligned sesamoids (the two small bones beneath the first metatarsal) to be repositioned. Further, the vertical bone cut allows for correction of a moderately-abnormal intermetatarsal angle by allowing the head of the metatarsal to be repositioned laterally. The metatarsal head can also be either elevated or lowered. This is not all, for with a small additional bone cut, the metatarsal head can be rotated in the sagittal plane--in a dorsiflexed or plantarflexed position to allow for repositioning of the cartilagenous surface. PASA can also be adjusted with another small bone cut. While interesting, versatile, and unique, this procedure is used rarely--only in cases where other procedures simply won't accomplish everything desired because this procedure is quite unstable compared to many other procedures. Still, it remains a useful tool when applied to the proper situations.
Hohmann Procedure Like the DRATO procedure, the Hohmann procedure is performed by making a vertical, trapezoidal cut in the bone, which allows for correction of a mis-aligned cartilagenous surface, as well as the correction of an enlarged intermetatarsal angle. The Hohmann procedure is considered unstable, and for this reason, other more-stable procedures are used much more commonly.
Shaft
Osteotomies
The procedures in this class are all designed such that a bone cut (osteotomy) is made in the region of the first metatarsal known as the shaft, or mid-portion of the metatarsal bone.
Most procedures in this class are designed to address an abnormality in the Intermetatarsal (IM) angle that accompanies most bunion deformities, the deviated cartilagenous surface (known as the PASA), or both.
Osteotomies performed in this region of bone are relatively slower-healing than a head osteotomy, however.
Vogler Procedure The bone cut is very
similar to the Kalish procedure described in the "head osteotomy"
section, but a Vogler or Off-Set V procedure is performed further back from the great toe joint.
Because the Kalish is performed in a quicker-healing area of bone, the
Vogler procedure is reserved more for patients with contraindications for
making a bone cut in that area, such as a cyst in the bone that doesn't
allow for firm screw fixation.
Peabody Procedure
The Peabody is basically the same as a Reverdin procedure (described
above in the "head osteotomy" section),
except that it is performed somewhat further back, away from the great toe joint.
The advantage of this is that it protects the joint surface and sesamoids
that lie to the bottom of the metatarsal, which can be compromised
by a true Reverdin. (This concern has been addressed with
modifications to the Reverdin procedure, however, like the Reverdin-Laird,
which we discussed in the Reverdin section above.)
Another advantage to this procedure is that it may be performed if there is
poor bone quality at the location where the Reverdin is usually performed.
The main disadvantage to this procedure is that
it heals more slowly than the Reverdin, so it is much less commonly
performed than the Reverdin procedure.
| Ludloff Procedure
This procedure entails an
oblique bone cut made diagonally through the first metatarsal as indicated
in the figure to the right. It allows
for nice correction of the IM angle and PASA, and this procedure also allows
the surgeon to lengthen and lower the metatarsal head.
The downside to this procedure is
that it is much more unstable than
procedures with interlocking pieces, such as the Kalish or Z-osteotomy,
(both described above). The
lack of interlocking pieces means that the Ludloff, unlike the
Kalish or Z-osteotomy, does not allow for walking immediately after
the procedure. For this reason, the Ludloff is not a
frequently-chosen procedure in the podiatric community except for
very specific applications. |
 |
Mau
Procedure Another oblique
osteotomy, this one made in the opposite orientation to the Ludloff.
Same advantages and disadvantages as the Ludloff. This procedure
is chosen even less frequently than the Ludloff because the ledge created by
this osteotomy is somewhat more
sensitive to the bone fracturing when weight-bearing is begun.
| Z-Osteotomy
Devised by a group of
podiatrists in Chicago, the
Z-osteotomy is similar to the Austin procedure, except that a Z-shaped bone
cut (as viewed from the side) is made instead of a V-shaped bone cut.
The "Z" may be made in either orientation, with the shelf
of bone on the top or on the bottom. You can see a diagram of
this procedure in the diagram to the right.
The Z-osteotomy is primarily designed to correct an abnormal intermetatarsal angle. The disadvantages to this procedure are that more soft-tissue dissection is required in order to make the bone cuts, and more bone is injured when making the rather substantial bone cuts. This causes additional damage to those tissues. It also doesn't address joint misalignment (PASA) too well because the interlocking pieces limit how much one can rotate the bone. Further, like the other procedures in this section, it is somewhat slower to heal. However, the interlocking
pieces afford this procedure great post-operative stability, so this
procedure is still chosen when great stability is required
post-operatively. |
|
A modification to the "Z" bunionectomy is the Scarf Procedure. A shortened version of the original Z-Osteotomy. This procedure is designed to allow for the additional stability of the Z-osteotomy, but diminish the amount of dissection required.
Mitchell Procedure
An old-time bunion procedure that used
to be a very commonly performed procedure. It can be used to correct the IM angle, though other procedures can correct the IM
angle to a greater degree. Some of its disadvantages are that there
are no interlocking
pieces like the Austin, Kalish, Reverdin, or Z-osteotomy, so it's quite unstable compared
to these newer procedures. It's also performed in a relatively
slow-healing portion of bone, and it's more difficult to fixate than other
procedures. Because of its disadvantages, and no real
advantages, the Mitchell
procedure is almost never performed in the podiatric community any longer.
Wilson
Procedure Another old-time
procedure designed to correct the IM angle. Like the Mitchell
procedure, the Wilson is rarely
performed today because of its instability and tendency towards slow
healing. There are no real advantages to this procedure compared
to newer surgeries.
Base Osteotomies
The procedures involving bone cuts in the base of the metatarsal bone have the big advantage over bone cuts made in the head or shaft of allowing for a greater amount of correction in severe bunion cases.
These procedures heal more
quickly than bone cuts made in the metatarsal shaft, too. However, these
procedures are inherently more unstable than the "head osteotomies"
discussed above, and typically require a cast and a period of non-weightbearing,
often a lengthy one. Hence, these procedures are typically used when the
amount of correction required outweighs the negatives of increased instability
during the post-operative healing phase.
| Closing Base Wedge
Osteotomy (CBWO) or
Louisan-Balacescu Procedure involves
removing the bump of bone on the metatarsal head, then making a
V-shaped piece of bone at the base of the first metatarsal.
With the V-shaped portion of bone removed, the pieces of bone are
put together, allowing the metatarsal to be straightened. (See
diagram to the right and below right for an x-ray of a completed
CBWO procedure.) |
Because the more stable "head osteotomies" (discussed above) can correct many moderate bunion deformities, this procedure is typically chosen to correct large IM angles. The disadvantages to this procedure are that screw fixation is difficult because of the orientation of the bone cut. In fact, due to the unstable nature of this surgery, it would be better (more stable) to insert two screws, but there's just not enough room with this bone cut. (See the Juvara Procedure below for how this can be overcome.) The other disadvantage to this procedure is that it shortens the first metatarsal, which is not always desirable. |
 |
Juvara Procedure The Juvara modification of the Closing Base Wedge Osteotomy involves the same basic type of cut as the CBWO, except the bone cut is made more obliquely across the shaft of the bone to allow for better screw fixation. In fact, two screws (to provide even more stability) can be inserted with the Juvara modification. Three versions of this procedure exist.
The Juvara A leaves an intact hinge for more stability.
The Juvara B is cut all the way through, leaving no hinge. This is less stable, but it allows the bone to be shifted downwards (plantarly) in cases where both the IM angle and an elevatus (an elevated bone) needs to be addressed.
The Juvara C consists of an oblique, through and through bone cut only. There is no wedge removed, so it is designed simply to allow the bone to be dropped. It can also be used to lengthen the first metatarsal somewhat.
Crescentic Osteotomy Also known as the Arcuate Osteotomy or Weinstock Procedure, this procedure involves a C-shaped bone cut made at the base of the first metatarsal. The advantage over the Closing Base Wedge and Juvara procedures is that there is comparatively no loss of bone length, as no wedge of bone is removed. The disadvantage is that the osteotomy is quite unstable. For this reason, this procedure is not done so frequently as the traditional Closing Base Wedge or Juvara procedures. Modifications can be made to this osteotomy, however, that improve the stability of this procedure.
When the patient has pathology at each end of the metatarsal, (like a very high IM angle that needs a base procedure to address along with a very deviated joint surface), the Crescentic procedure may be coupled with a Reverdin, Austin or some other head procedure.
Opening Base Wedge Procedure (Trethoan) The Opening Wedge Osteotomy involves making a cut in the base of the first metatarsal and inserting a V-shaped piece of bone on the side of the first metatarsal to address the Intermetatarsal angle. The advantage of the procedure is that it doesn't remove bone, which wouldn't be advised in patients with already short first metatarsals. Indeed, it adds bone. But you need to use a bone graft for this procedure, and it is very slow healing, requiring a cast and twice as much time off the foot as a Closing Base Wedge or Crescentic procedure.
Proximal Chevron First appearing in the medical literature in 1929, the Proximal Chevron is actually the first V-shaped osteotomy described in the medical literature, but it has only recently begun to enjoy a resurgence since modern screw fixation has made this procedure practical.
It involves making the same V-shaped bone cut as the Austin
procedure (described above), only making the bone cut at the base of the first
metatarsal. This procedure allows more correction than the traditional Austin
procedure, and is somewhat more stable than the other procedures in this
category.
Procedures
Proximal to the First Metatarsal
| Lapidus Procedure The Lapidus procedure has become more popular over the past ten years or so. It involves the fusing of the first metatarsal bone with the midfoot (specifically, the first cuneiform bone). The idea with this is that the deformity of the increased intermetatarsal angle is based at this joint, so fusing this joint will stabilize the bunion. Typically screws or a plate is used to hold the bones together. Sometimes the Lapidus is performed with additional fusions of other joints in particularly hypermobile feet. A particularly good procedure for very flexible individuals and for younger patients who are prone to quicker return of bunion deformities. Drawbacks include its slow-healing nature, its need to be immobilized and non-weight bearing for lengthy periods of time, and the fact that it shortens the first metatarsal. |  |
Stamm Procedure (Opening
wedge in first cuneiform) Instead
of removing a piece of bone to allow the intermetatarsal bone to be
corrected, this procedure allows for adding a wedge of bone in the cuneiform
to effect the same purpose. Its drawbacks are that it is even more
slow-healing than a Lapidus, requires a graft, and must be kept non-weight
bearing for a long time while the graft incorporates into the
bone.
Joint Salvage Procedures for Arthritis
This class
of procedures is chosen when there is a substantial amount of arthritis in
the big toe joint, but an attempt is made to keep the natural
joint. (If you're interested in this category of procedures, you
may wish to visit our web page for
hallux
limitus and hallux rigidus, as well.)
Bonney-Kessel Procedure In cases with severe arthritis, this procedure can be chosen to permanently bend the bone in the great toe. In theory, this allows the patient to roll forward off the bent toe, without causing excessive painful bending the big toe joint.
Waterman Procedure Similar to the Bonney-Kessel, the Waterman involves a bone cut made in the first metatarsal instead of the big toe. This procedure helps decompress the arthritic great toe joint, and it also may serve to help rotate healthier cartilage into an arthritic great toe joint.
Cheilectomy See details under the heading Bump Removal Procedures above.
Lambrinudi Procedure The Lambrinudi procedure was described primarily to drop an elevated 1st metatarsal, thereby addressing hallux limitus and hallux rigidus. But it may be performed in such a way to address an increased intermetatarsal angle, as well. It basically consists of a similar bone cut to a Ludloff, except a second bone cut is made to create a pie-shaped wedge. When the triangular-shaped piece is removed, the bone is able to "plantarflex," or drop. Screw fixation is relatively easy with this procedure. The same downsides exist for this procedure as with the Ludloff.
Giannistras Procedure The Giannistras is a Z-shaped bone cut that allows the bone to be shifted up or down (most frequently). It doesn't correct an increased IM angle, however. This procedure is rarely done because it requires a fair bit of tissue dissection and because it is relatively unstable compared to other procedures.
Youngswick
Procedure One of the most
popular procedures in the podiatric community to decompress an arthritic toe
joint, the Youngswick is a modification of the Austin (Chevron) procedure
that allows the metatarsal head to be lowered and shortened when this is
desired. See the details under the
heading Head Osteotomies above
for more information on this procedure.
Joint Destructive Procedures
These
procedures are performed only when there is a great deal of arthritis in the
big toe joint, and the joint is no longer salvageable. (If you're
interested in this category, you may wish to visit our web page for
hallux
limitus and hallux rigidus, as well.)
| First Metatarsophalangeal Joint Arthrodesis This involves fusing the big toe joint. Fixation for this procedure may be accomplished through screws, pins, and plates. This procedure may be useful when there is severe pain due to arthritis, and it can be done to address the intermetatarsal angle as well. There are a few downsides to this procedure. The first is that this procedure is relatively slow healing, which makes it more commonly performed on somewhat younger individuals as those in the older age category may have a difficult time healing from this procedure. Second, there is no toe motion after it heals, which not only can be annoying for some people, it will also alter one's gait, which can make walking uncomfortable in other locations throughout the foot, ankle, and body. |  |
Hueter Procedure Involves the removal of entire metatarsal head. Because this bone normally bears a lot of weight, this procedure is almost never performed, except in severe cases of arthritis, trauma, infection, or other exceptional circumstances. More of a historical procedure.
Mayo Procedure Similar to the Hueter, except that it removes a smaller portion of the metatarsal head. It is also like the Hueter procedure in that it is not frequently chosen in the podiatric community.
Implants Metal and silicone implants exist and may be implanted in cases of severe arthritis. They tend to need replacement, often after 10 years or so, and this requires a second surgery. At that time the patient may need another implant, a joint fusion, or a Keller procedure.
Keller Procedure (First Metatarsophalangeal Joint Arthroplasty) Well over 100 years old, this procedure involves removing the base of the big toe and (usually) inserting soft tissue to separate the remaining bone. At one point this procedure was done almost indiscriminately on virtually anyone with a bunion deformity. Today it is reserved for those with severe arthritic joint disease where other treatments are not advised. |
 |
Advantages to this procedure is that it allows for immediate weight bearing after the surgery, and it results in a large increase in pain-free motion. Further, it heals very quickly, much more so than the other procedures in this category.
The downsides to this procedure are that the patient loses push-off power of the big toe, and the big toe looks a little short aesthetically. Because this procedure shortens the big toe, some people will get some discomfort in the ball of the foot afterwards that may need an innersole or orthosis to control.
Valenti "V"
resection A modification of the
Keller procedure. It involves taking an angular piece of the top of the
big toe and the first metatarsal to increase range of motion.
Soft Tissue Procedures
These procedures are almost never done by themselves, as they don't address the abnormal bone that is almost always present with a bunion deformity. However, these procedures are frequently performed along with a primary bunion procedure to augment the main procedure.
Hiss Designed to be done on its own, this procedure involves a tendon balancing to help pull the big toe straight. Procedures involving bone cuts work much better, so this procedure is rarely done, and more of a historical procedure.
Adductor Transfer This procedure is designed to address the tendon that pulls the big toe abnormally towards the second toe (common with bunion deformities). This tendon is known as the Adductor Hallucis Tendon, and it may be detached from the great toe (allowing it to better straighten) and reattached to the sesamoids to straighten them back onto the metatarsal. It is only done adjunctively, or as part of a larger procedure that includes making bone cuts.
Lateral release Alternative to the Adductor Transfer procedure, the Adductor Hallucis Tendon can simply be cut from the big toe bone, without attempting to reattach it to straighten the sesamoids. Again, done as an adjunctive procedure.
Capsulorraphy When a bunion has existed for a long period of time, the covering to the big toe joint over the bump often becomes stretched. A capsulorraphy procedure involves taking a wedge of tissue from the stretched capsule to tighten it up. This, too, is done as an adjunctive procedure.
Sesamoid mobilization When the sesamoids have become scarred down from being misaligned so long, they can be loosened from their soft-tissue contracture via a mobilization procedure. Usually done as an adjunctive procedure.
Sesamoid removal When the sesamoid(s) are so diseased to function normally, one--or rarely both--of the sesamoids may need to be removed. This may be done as an isolated procedure for a sesamoid fracture or other non-healing injury or adjunctively in combination with a bunion surgery.
EHL Tendon Lengthening The Extensor Hallucis Longus Tendon (a tendon that pulls your toe upwards) can sometimes be a deforming factor in a bunion deformity. It may need to be lengthened or altered in one of several possible ways to address this. This is usually an adjunctive procedure.
Tendon Transfer
Several
tendons may be transferred in a bunion procedure. We've already
discussed the Adductor Hallucis Tendon above, but the Abductor Hallucis,
Extensor Hallucis or Flexor Hallucis Tendons may also be transferred on
occasion. This may be done as an isolated procedure in rare
cases, but it is usually done in combination with a procedure involving bone
cuts.
Digital Procedures
Procedures performed in the big toe are typically too far distal (forward from the bunion) to truly correct the major portion of a bunion deformity. For this reason, these procedures are usually adjunctive procedures, done as part of an overall reconstructive procedure involving both the metatarsal and an abnormally-oriented great toe. These procedures are not frequently done in isolation.
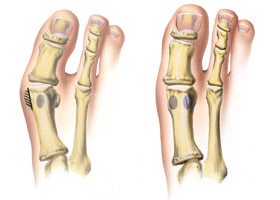
Akin Procedure Another very old procedure, the Akin remains the best known and most frequently chosen procedure in this group. While once described as the primary procedure to address a bunion, it is now very rarely done in isolation. Rather, it lives on mostly as an adjunctive procedure to add to a bunion surgery when the great toe is bowed.
The Akin involves taking a wedge of bone out of the great toe bone and reorienting the bone.
The bone cut is typically made where the deformity in the bone is most pronounced. For example, the Proximal Akin involves removing a wedge of bone from the base of the first big toe bone. (This would be represented by the lower bone cut on the diagram to the right.) A Distal
Akin is the same procedure performed
farther from the toe joint and closer to the toe nail. This is
demonstrated in the upper bone cut on the diagram to the
right. |
|
| An Oblique Akin is performed with the wedge of bone removed in an angular fashion diagonally across the first great toe bone. The example of the Distal Akin above is an oblique bone cut. Oblique bone cuts are typically made to allow for screw insertion. An example is represented by the angled bone cut on the top of the diagram to the right. |  |
A Cylindrical Akin shouldn't really be called an Akin at all, as there is no wedge of bone removed. Rather, this procedure involves making a curved cut in the base of the first big toe bone, thereby allowing the rest of the toe to be realigned. The advantage of this procedure is that there is no bone removed in the procedure, so it shortens the big toe less than the other Akin procedures above. The disadvantage is that it is less stable post-operatively, and really needs excellent fixation.
Schumacher Procedure This procedure was devised by Dr. Schumacher to straighten the great toe like an traditional Akin, but with the advantage of not removing any bone--just as the Cylindrical Akin does. This procedure allows the correction to be achieved without shortening the big toe--in fact in can be lengthened slightly. The advantage over the Cylindrical Akin is that it is more stable post-operatively. The disadvantage is that somewhat more soft-tissue dissection is required than with either the traditional Akin or the Cylindrical Akin.
Regnauld Procedure This
procedure is designed specifically to shorten an excessively long big
toe. Not frequently performed, as there are other, technically easier ways to accomplish
this goal.
Combination Procedures
Logroscino
Procedure This
procedure is a Closing Base Wedge Osteotomy (CBWO) (described in the Base
Osteotomies section) to close down an enlarged
intermetatarsal angle, coupled with a Reverdin procedure (described in the Head
Osteotomies section) to reorient the
cartilage.
Stamm Procedure
Discussed above in the
Procedures Proximal to the First Metatarsal
section, this procedure is basically an Opening Base Wedge Osteotomy (OBWO), (see
details under the heading Base
Osteotomies) to correct an enlarged
intermetatarsal angle, with a Keller procedure added to remove a severely
arthritic joint (see details under the heading Joint
Destructive Procedures).
While these are two examples of "combination" procedures, there are actually dozens of other procedures, especially when you consider all the possibilities just from combining two or three of these procedures to address multiple abnormalities.
Some of these combinations are named after people like the two listed above. Others are simply the original names of the procedures combined with hyphens. For example, one could choose an Austin-Keller, a Youngswick-Akin, a Reverdin with a Medial Capsulorraphy, and so forth.